Editor’s note — Highland County Health Commissioner Jared Warner posted an update focusing on COVID-19 on the health department’s Facebook page Wednesday. The slightly edited update appears below:
Cases
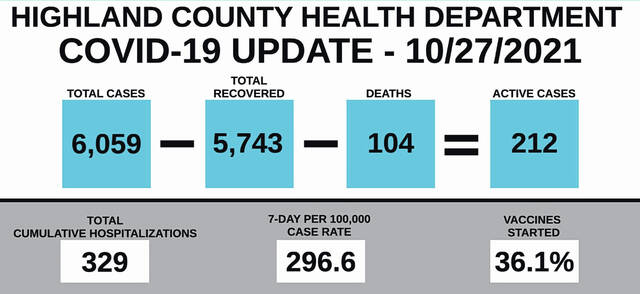
Case counts have increased slightly over the past few days, putting Highland County at 296.56 on a seven-day per 100,000 population average. This means that we are seeing about 17 new cases each day on a seven-day average. This slight increase was also seen in Clinton and Brown counties. Could this be a result of our colder weather this week? Maybe something to do with some new sports seasons starting up resulting in new gatherings of different people? There is no way to know for sure, but we are watching this increase closely and hoping that it is just a temporary increase.
Highland County also saw its COVID-19 deaths increase to 104 this week. Anecdotally, I had a local funeral director say to me that he had seen a lot of COVID-19 deaths in the last several days, so we may see additional death numbers added soon.
Hospitalizations seem to be slowly decreasing still, with 329 cumulative hospitalizations to date. Regional hospitalization numbers are still slowly declining, but ICU capacity remains a problem (not all because of COVID).
Vaccination rates are at 36.1 percent for our county population.
Vaccine boosters
There is a lot of information to unpack with the FDA and CDC vaccine booster approvals that came out late last week. Here are the highlights and I encourage anyone who wants more detailed information to visit the CDC website to read the recommendations in full. The details can be confusing.
Booster vaccine doses are approved for Moderna, Johnson and Johnson and Pfizer vaccines.
For Moderna and Pfizer, boosters are approved for the following groups as long as it has been at least six months since your initial vaccine series was completed: Those over 65, over 18 with underlying medical conditions, over 18 who live in long-term care settings, and over 18 who work or live in high-risk settings.
Moderna’s booster doses are half of the initial dose size, while Pfizer is at the same dose size. A “third dose” of Moderna or Pfizer is different than a booster (yes, this is very confusing), and it is intended for people who are immunocompromised. Third dose vaccines are all given at the normal full dose size.
Johnson & Johnson is a little different. CDC has approved J&J vaccine boosters for anyone over the age of 18, so long as it has been at least two months since the initial dose. J&J boosters use the same amount of vaccine as the initial dose.
Late last week, the CDC and FDA also approved the mixing of vaccines for booster doses. This means that people can choose any type of vaccine for their booster dose. Some people may decide to change brands of vaccine for their booster, but the health department is not able to provide any individual recommendations on what brand to get as a booster.
School quarantine procedures
The Ohio Department of Health announced new K-12 school quarantine procedures that school boards have the ability to adopt as a way to limit the impact of quarantine in school systems and to keep kids in school. We have been watching this topic closely over the past few months and discussing this option with our local school systems in preparation for this shift.
Essentially, the new policy allows students and staff who are exposed to COVID-19 in a school setting to stay in school provided that they follow some specific guidelines. These guidelines are as follows (copied from ODH policy):
Mask to stay/test to play option
Quarantining students at home who have been exposed to COVID-19 in a school environment has the unintended consequence of reducing in-school learning and can be an added strain on parents, schools and local health departments (LHDs). While vaccination and mask usage are critical components to ensuring a safe school environment, we offer an in-school alternative to quarantining students and school staff at home who have been exposed to COVID-19 in a school environment to support in-school learning and reduce the strain.
This recommendation is informed by a growing body of national experience, a pilot in Warren County and experience shared by other LHDs that points toward a low number of individuals with direct contact to a COVID-19 positive individual within a school setting who convert to positive cases. Based on this information and the success of the Warren County pilot, we recommend the following for K-12 students and staff exposed to COVID-19 in a school setting.
Please note: Eligibility to participate in mask to stay/test to play is contingent on the exposure being in the school setting or school-related activities. This does not apply to household exposures or exposures outside of the school setting or school-related activities.
Mask to stay
Direct contacts, regardless of vaccination or masking status, may remain in the classroom environment if they do the following: Wear a mask for 14 days after their last date of exposure, self-monitor or parent-monitor, for symptoms of COVID-19; isolate and get tested if they start to experience symptoms associated with COVID-19 (regardless of the level of severity); consistent with guidance for others quarantining in lower-risk environments, students and staff may discontinue these quarantine procedures after seven days, if they don’t develop symptoms and test negative between days five to seven.
For extracurricular activities, ODH provides the following policies:
Test to play
Asymptomatic contacts may continue to participate in extracurricular activities if they do the following: Wear a mask when able (this includes: transportation; locker rooms; sitting/standing on the sidelines; and anytime the mask will not interfere with breathing, the activity, or create a safety hazard; test on initial notification of exposure to COVID-19; test again on days five to seven. If they are negative at this time, they will test out of quarantine.
These are new policies, and there are lots of questions that we still have about how to apply this locally if our schools adopt this approach.
There are also some things about the policy that don’t make sense to me, like the requirement for wearing a mask for 14 days while in school. Students that choose to do a 10-day at home quarantine can come back without a mask after quarantine, but this in-school policy requires a 14-day mask time frame.
The policy also calls for immediate initial testing for students who want to participate in sports, but we know that testing someone immediately after their exposure is very, very unlikely to result in a positive test because the viral load of the person is unlikely to be high enough to test positive. Sometimes we find out about an exposure very quickly, and other times it might be several days after exposure before we find out about a case. A blanket “test immediately” approach doesn’t make sense.
Maybe the largest inconsistency is that individual close contacts in sporting events and other extracurricular activities will not be notified or quarantined individually. Instead, the entire team will be notified as a whole about the exposure, but the team will not be required to follow the “mask to stay” policies because of the exposure. This makes little sense as contacts that occur during sporting events are often much, much closer than contacts that might occur in a classroom setting.
This new policy is likely to be a useful tool for our schools, but we need to remember that it is very new and there are still lots of questions and clarifications that we will need to talk about along the way. I have also asked the schools to also think about how this policy might work in times of high risk. Right now, our cases counts are fairly low, and risk is low as a result. It may be difficult to use a “mask to stay and test to play” approach if we see a significant spike in cases again. Highland County’s child vaccination rate is also very low, which can also impact how effective a strategy like this might be.
Risk and behavior
I keep working on finding the right analogy to help visualize how we already adjust our behavior based on risk levels in our normal life. We need to get more comfortable doing this for COVID-19 as well. Here is my latest attempt at an example that will help make sense of this idea.
When do we put salt down on the road? We salt the road in the winter when it is cold enough to be slick and the forecast calls for snow or ice. We don’t salt the roads in the summer when the sun is shining and the weather is warm. Our COVID-19 policies need to follow the same mindset. When the risk is higher during a COVID-19 case surge, our community needs to support adding some additional temporary layers of protection. This might include being more cautious in our schools, bringing masking back into our businesses and schools, changing our social activities and making other changes to help reduce how many people get sick.