Local and state health officials are still struggling to keep up with new COVID-19 cases and quarantines, Highland County Health Commissioner Jared Warner reported in a Friday post to the health department’s Facebook page.
Last week, the Highland County Health Department implemented an automatic survey to assist with contact tracing so health department staff could focus on high-risk cases.
Warner reported Friday that over the last three days, health department staff made over 300 phone calls and sent over 200 letters.
Due to the volume of new cases, Highland County residents who are confirmed to have COVID-19 should not wait for the health department to contact them but should isolate at home for at least 10 days. After 24 hours without a fever and “a great improvement of symptoms,” residents may exit isolation, Warner said.
The Ohio Department of Health (ODH) is dealing with similar issues, Warner said. As of Friday, the ODH added a note to its COVID-19 dashboard which reads, “Today’s data is incomplete; thousands of reports are pending review.”
Health officials continue to express concern for the increased number of COVID-19-related hospitalizations and hospital capacity.
On Wednesday, Warner reported that the number of COVID-19-related hospitalizations is greater than the number of hospitalizations during recent flu seasons.
During the past two flu seasons, 27 people and 38 people, respectively, were hospitalized due to influenza; from March to Nov. 20, 59 people were hospitalized due to COVID-19.
On Friday, Warner addressed a question he received this week regarding the state’s hospitalization rates.
“I received the following question earlier this week,” Warner wrote, “and I think it is a very legitimate question to ask: ‘Are the hospitals really in as bad a shape as our infamous governor says? Or is this an exaggeration to curb future problems?’
“The short answer is yes, and yes.
“The long answer to this is complicated, so let’s break it down into a few parts. The healthcare system has a few constraining factors that can limit their ability to keep patients and staff safe and provide the standard of care that we expect.
“Staffing — Healthcare staffing can be a significant limitation for healthcare response to pandemics. Hospitals often run at 80-90 % capacity in a normal year, and they have staff on payroll to meet this normal need. This includes elective surgeries, short term stays, recovery for minor procedures, etc. Being 80% full on a normal year may not be the same as 80% full if a majority of cases are infectious diseases. Percentages only tell part of the story here.
“Additionally, when we start increasing our overall hospital usage, it can be difficult to find staff to support increased bed usage. Combine this with staff who are often getting sick themselves, and we can run into staff shortages pretty quickly. Hospitals run on people, not beds, so this is something that we are really concerned about.
“Personal Protective Equipment (PPE) — PPE supplies are much better than they were early on in this pandemic. When we have increased COVID-19 cases, healthcare staff use significantly more PPE supplies than with non-COVID-19 patients. This can begin to cause a strain on supply issues over the long term. I have heard reports of inventory shortages and order delays already occurring. Lack of available PPE leads to less well-protected healthcare workers, which can reduce the number of beds that can be staffed for COVID-19 patients.
“Beds — Bed availability is something that can fluctuate greatly depending on several factors and decisions made by the hospital. Hospitals can postpone elective surgeries in order to free up beds and staff, but this is not a long-term solution. Eventually, these postponed procedures will need to be done. Alternative areas in the hospital can be developed in order to provide additional bed capacity, but this can reduce the level of care available to patients. In short, hospitals can flex their capacity quite a bit, but there are tradeoffs.
“Current Situation — Current hospitalization trends are all headed up sharply. This is creating strain on staffing resources and PPE currently, and can lead to general hospital capacity issues down the road. Several hospitals in our urban centers have reached very high levels of bed use. One hospital has added an outdoor tent for ED overflow. Others have already started to limit elective procedures that require an overnight stay. Things are not great currently in our healthcare systems.
“Governor DeWine is calling attention to this problem because it already is an issue. We have to remember a couple of important things. First, hospitalizations are a lagging indicator. Hospitalizations will rise a week or two after any large surges in cases, which means that any policy changes that we make today will take several weeks to make an impact on our numbers.
“It reminds me of my short career driving a water truck for the City of Lebanon. I learned the hard way that you have to start braking early in order to slow big heavy things down. We have to raise the alarm now because our current COVID-19 trends show us where we are headed.
“I will include a couple of charts that demonstrate the current trends. This isn’t cause for panic, but we need to be thinking ahead and making changes while we are still able to apply the brakes.”
The following are Highland County’s overall COVID-19 statistics as of Friday:
Highland County has had a total of 986 lab-confirmed and probable COVID-19 cases, according to the Highland County Health Department.
The health department reported that there were 158 actively sick patients and five COVID-19-related hospitalizations, and the health department is monitoring 380 Highland County residents for symptoms.
Since the COVID-19 outbreak reached Highland County, there have been a total of 59 COVID-19-related hospitalizations and 19 COVID-19-related deaths, and 809 patients have recovered from COVID-19.
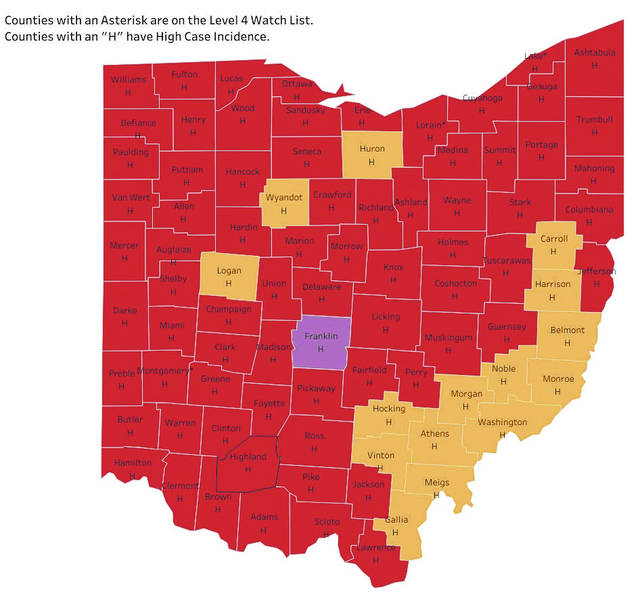
As of Thursday, Highland County remained a “red” county with high case incidence, according to the Ohio Public Health Advisory System (OPHAS).
“Red” counties, which OPHAS also classifies as level 3 public emergencies, have “very high” COVID-19 exposure and spread.
Highland County currently has a rate of 417.04 new cases per 100,000 residents, Warner reported on Friday.
Out of Ohio’s 88 counties, 72 counties were rated as “red” counties; 15 counties were rated as level 2 “orange” counties.
Franklin County became the first level 4 “purple” county, which designates severe exposure and spread. Those in “purple” counties residents should only leave home for essential supplies and services.
No counties were rated as level 1 “yellow” counties, the lowest rate of exposure and spread.
According to the ODH, which reported 882 cumulative cases in the county as of Thursday, of the cases in Highland County:
* 142 cases involved 50- to 59-year-olds. Of these cases, nine resulted in hospitalization.
* 133 cases involved 60- to 69-year-olds. Of these cases, 10 resulted in hospitalization, and two resulted in death.
* 121 cases involved 40- to 49-year-olds. Of these cases, six resulted in hospitalization.
* 120 cases involved 70- to 79-year-olds. Of these cases, 19 resulted in hospitalization, and five resulted in death.
* 107 cases involved 20- to 29-year-olds. Of these cases, one resulted in hospitalization.
* 97 cases involved 0- to 19-year-olds. Of these cases, one resulted in hospitalization.
* 91 cases involved 30- to 39-year-olds. Of these cases, one resulted in hospitalization.
* 69 cases involved someone 80 years old or older. Of these cases, 12 resulted in hospitalization, and 10 resulted in death.
* Two cases involved patients of unknown ages.
Warner previously stated that there is a delay in the reporting process between individual counties and the ODH.
Reach McKenzie Caldwell at 937-402-2570.